The tough science behind locating breast tumours
3 May 2024
Breast tissue has an unnerving tendency to move around in complicated ways, making it hard to pinpoint breast tumours when it comes to surgery. A team at the Auckland Bioengineering Institute wants to change that.

When Robin Laven bought a coffee machine off TradeMe recently, it didn’t take long before he discovered he and the seller had something in common: a commitment to beating breast cancer. The seller was just recovering from surgery; Robin's research at the University of Auckland is trying to improve outcomes for breast cancer patients.
That was far from the first time his job and his life have intersected.
“I’m always surprised at the number of people I come across impacted by breast cancer.”
Robin is a PhD student at the Auckland Bioengineering Institute (ABI). His work involves developing specialised camera equipment to help build 3D images of someone’s breast so doctors treating and removing tumours can accurately pinpoint where those tumours are.
It sounds strange. Surely mammograms, MRIs and other scans can do that already?
But what most people don’t know, Robin says, is one reason why treating breast cancer is so notoriously difficult, is that breast tissue moves around in complicated ways. And because a tumour might be only a millimetre or two in size, any change in perceived position can make them hard to find.
A surgeon might miss some or all of the cancerous tissue.
You can get a lot of surprisingly complicated movement within the breast, which makes it hard to predict where the tumour is.
Think about it like this, Robin says. During a mammogram, the breast is squashed: radiologists spread out the tissues to get the best image. On the other hand, people typically get a breast MRI lying face down.
And when it comes to surgery, of course, the patient will be lying on their back, with the breast in a very different shape and position.
“Between these positions, you can get a lot of surprisingly complicated movement within the breast, which makes it hard to predict where the tumour is,” Robin says.
This has big ramifications. One in nine New Zealand women will be affected by breast cancer in their lifetime, according to the Breast Cancer Foundation. That’s 3300 women diagnosed with breast cancer each year, and 25 men. More than 650 people will die from the disease annually.
Surgery is the first breast cancer treatment for more than 90 percent of people in Aotearoa, a 2022 Breast Cancer Foundation report said. And around 20 percent of women need a second surgery, which can be tough. Some of these breast cancer re-operations are due to difficulty accurately pinpointing the tumour, Robin says.
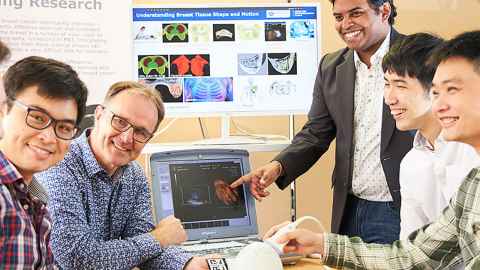
Robin is part of the ABI's Breast Biomechanics Research Group, which is led by Professor Martyn Nash, Professor Poul Nielsen, Dr Gonzalo Maso Talou, and Dr Thiranja Prasad Babarenda Gamage.
The goal for the team is to build biomechanical models of the breast using its various components and “a bunch of mathematical equations”, Robin says.
This personalised ‘digital twin’ model, made from their images, should make it easier to see how breast tissue might move under various conditions, and therefore help surgical teams predict where a tumour might be.
Robin’s own PhD is tracking the surface of the breast. Using five cameras he can build 3D images of the way that surface moves from different angles and with someone’s arms and body in a variety of positions. He can then build that into the digital twin model.
“If we can measure and track this skin surface motion it will help us fine tune our predicted tumour locations," he says.
"In the future we want to get to a situation where as someone moves, we can actually update our estimate of where the tumour is inside the breast in real time. And that will basically give doctors up-to-the-second targeting information for where these tumours are.”
Until now Robin, has designed and developed the workings of his camera technology in the lab. The next stage is a “very small trial” – one woman and one man.
The group also has a larger study planned with about 20 people.
If we can measure and track this skin surface motion it will help us fine tune our predicted tumour locations.
The hoped-for outcome is to be able to build personalised digital twins without the need for an MRI, so more people can benefit from personalised medicine.
Robin sees the work the ABI Breast Biomechanics Research Group is doing as complementing, rather than replacing, existing technology.
“MRIs are super-powerful as an imaging technique, but it can be difficult to get multiple images,” Robin says. “When radiologists are scanning someone, they are really trying to get the best possible images for finding tumours, but this comes at the cost of knowing exactly where the tumour will be during surgery.
Also MRIs are expensive and mainly available in bigger hospitals, and hence generally limited to main centres.
“I hope this line of research will help to provide a platform for making these predictive models cheaper and more widely available, allowing them to be built from ultrasound and cheap handheld devices, as opposed to MRI or CT scans.”
Media contact
Nikki Mandow | Research communications
M: 021 174 3142
E: nikki.mandow@auckland.ac.nz