Breakthrough offers hope for aggressive leukaemia
5 June 2024
Scientists are excited they may have found a new way to treat acute myeloid leukaemia that could be more effective and have fewer side effects than current treatments.

Researchers at Waipapa Taumata Rau, University of Auckland are working on an innovative way to treat an aggressive blood cancer, called acute myeloid leukaemia.
Acute myeloid leukaemia is the most common type of acute leukaemia in adults in New Zealand, affecting around 150 people per year, but current treatments haven't changed much since the 1970s.
“While there have been some successes with treatments, such as vitamin A and arsenic trioxide, they have worked for only a very small number of patients with very specific genetic changes,” says Professor Stefan Bohlander, co-director of the University’s Leukaemia and Blood Cancer Research Unit.
“The remaining patients have genetic changes that are quite complicated, making treatment difficult.”
Acute myeloid leukaemia affects the blood and bone marrow, which is where blood cells are made. It makes the body produce an excessive number of abnormal white blood cells, which interferes with the production of healthy blood cells.
“Current treatments, like strong chemotherapy and bone marrow transplants, can be very tough on patients and don't always work well, especially for older people,” says Dr Bohlander.
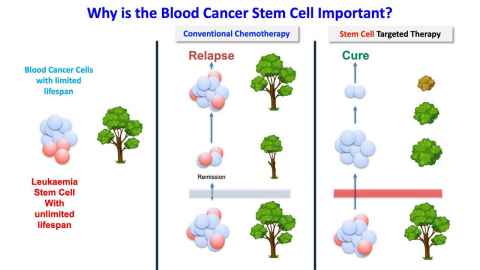
Scientists have found that a small group of cells, called leukaemia stem cells, are a big part of the problem.
“The current treatments do not specifically target the stem cells but all cells indiscriminately, and that's why they are very toxic and frequently do not lead to cure,” Dr Bohlander says.
It's been very hard to find a way to target and destroy these cancer-causing stem cells without harming the healthy stem cells the body needs, says Dr Bohlander.
Dr Alyona Oryshchuk, who did her doctorate at the University of Auckland, made an exciting discovery. She found that a specific inhibitor can get rid of leukaemia stem cells in a mouse model of leukaemia, while protecting the healthy stem cells.
This means there might be a new way to treat acute myeloid leukaemia that could be more effective and have fewer side effects.
This research project, led by Professor Bohlander, Professor Peter Browett, and Dr Purvi Kakadiya, has received funding of $350,000 over three years from Leukaemia & Blood Cancer New Zealand, as part of their longstanding commitment to funding the Leukaemia and Blood Cancer Research Unit.
They hope to prove that Dr Oryshchuk’s discovery can work in other leukaemia models too.
Dr Oryshchuk is thrilled to continue her research and work with other scientists. She presented her findings at a major international conference in Australia, where they were well received.
This research could lead to new treatments that help more people with acute myeloid leukaemia survive and live healthier lives.
Media contact
FMHS media adviser Jodi Yeats
M: 027 202 6372
E: jodi.yeats@auckland.ac.nz