Vulnerable babies and children benefit from new ABI research funding
5 December 2024
Research into perinatal brain injury and new tools for paediatric surgery has earned Sir Charles Hercus Health Research Fellowships for two rising stars at the Auckland Bioengineering Institute.
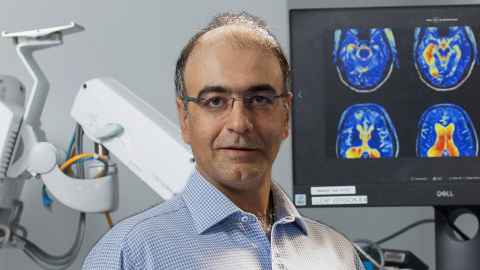
Dr Hamid Abbasi will receive $600,000 for research on using AI technology to detect perinatal brain injury.
His project aims to revolutionise care for newborns affected by hypoxic-ischemic - a devastating brain condition caused by oxygen and blood flow deprivation during birth. This condition impacts between 50-70 newborns annually in New Zealand alone, and often leads to lifelong neurodevelopmental challenges.
The project focuses on leveraging cutting-edge artificial intelligence and advanced high-resolution EEG biomarkers to precisely determine the timing and severity of brain injury within the critical six-hour "golden window" after birth.
The aim is to develop real-time diagnostic tools for bedside use, ensuring timely and life-saving interventions – particularly for high risk populations such as Māori preterm infants. The project will help prevent lifelong disabilities, improve quality of life, and significantly lower healthcare costs.
Better lives for young patients
Dr Julie Choisne will receive $599,601 for research on implementing biomechanics tools for paediatric surgery.

Conditions such as hip dysplasia and cerebral palsy can lead to complex deformities in young patients. Because these bone deformities affect each child differently, doctors find it hard to predict which surgeries will work best for each individual child.
To solve this problem, Julie aims to create personalized medical solutions using advanced technology that can predict children's unique body structures. She has already developed computer models using medical scans from healthy children aged 4 to 18 - the next step is to test these models using medical images from children with bone deformities.
By creating these personalized healthcare tools for orthopedic medicine, she hopes to develop more precise treatments that can significantly improve patients' lives and delay possible complications in adulthood such as osteoarthritis.
These two Fellowships are part of $7.78 million the Health Research Council has awarded to University of Auckland researchers.
Media contact
Nikki Mandow | Research communications
M: 021 174 3142
E: nikki.mandow@auckland.ac.nz